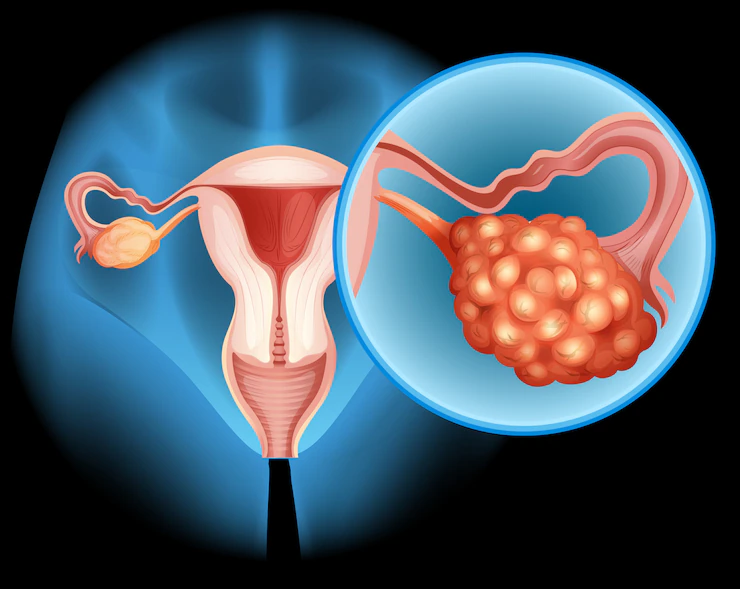
A solid or fluid-filled region in or on your ovary is called an ovarian cyst. They are typical, particularly in young or pregnant women who have not yet reached menopause. They are often innocuous and painless. Without realizing it, you could experience one each month as part of your menstrual cycle. Usually, they disappear without any medical intervention.
When a cyst doesn’t go away or worsens, it becomes an issue. It may grow uncomfortable. Cancer is also a possibility, but it’s uncommon. As you age, your odds increase.
Symptoms of ovarian cysts
The majority of ovarian cysts are tiny and asymptomatic. You may have pressure, bloating, swelling, or pain on one side of your lower abdomen when you have symptoms. This discomfort might come and go and be either intense or dull.
Sometimes a cyst requires immediate care. When you experience any of the following:
- menstrual cycle changes unusual vaginal bleeding
- pelvic pain
- a dull pain in the lower back and thighs that occurs soon before the start or conclusion of menstruation.
- discomfort during having sex, discomfort passing a stool, pressure on the bowels, or frequent bowel movements
- problems full bladder emptying or frequent urination
- sudden weight gain
- breast sensitivity
Ovarian cyst causes and types:
Ovarian cysts can have many different causes, and the majority of them are not malignant.
Follicular cysts: A follicular cyst is the most prevalent form and develops as a follicle grows. The typical fluid-filled sac that houses an egg is called a follicle. When the follicle expands beyond normal size throughout the menstrual cycle but does not open to deliver the egg, follicular cysts develop. Follicular cysts typically go away on their own over days to months. Hemorrhagic cysts in the follicles might develop as a result of blood leaking into the egg sac.
Corpus luteum cysts: The menstrual cycle is associated with corpus luteum cysts. The ovary’s corpus luteum is a region of tissue that forms after an egg is discharged from a follicle. The corpus luteum often disintegrates and vanishes if a pregnancy doesn’t take place. On the ovary, it may, however, continue to grow as a cyst after filling with liquid or blood. This cyst often only affects one side, exhibits no symptoms, and disappears on its own.
Chocolate Cysts: Cysts made of chocolate endometriosis is a conditions in which cells that ordinarily line the uterus (womb) outside the uterus instead line other parts of the body. Endometriosis commonly affects the ovary. When endometriosis affects the ovary, the affected endometrial tissue may swell and bleed over time, developing into an endometrioma, often known as a “chocolate cyst,” which is a blood-filled cyst with red or brown contents.
Ovarian polycystic syndrome: Multiple tiny cysts in both ovaries are a defining feature of polycystic ovarian syndrome (PCOS) disease. PCOS is the most prevalent hormonal condition that leads to infertility in women and is linked to several hormonal issues.
Tubo-ovarian abscesses: The ovaries and Fallopian tubes may get infected along with other pelvic organs. On, inside of, or around the ovary or tubes, there may be pus-filled cystic areas in extreme cases. The term “tube-ovarian abscesses” refers to this.
Diagnosis of an ovarian cyst
Cysts can be mixed, solid, or fluid-filled. Your doctor might suggest one or more of the following tests determine which type you have:
- Pregnancy test.
- Abdominal ultrasound.
- Laparoscopy.
- Blood test for CA 125.
Treatment for Ovarian Cysts
Cysts typically disappear on their own. Your doctor might advise keeping an eye out for any changes.
You can receive pain medication from your doctor. Additionally, they could recommend birth control medications. The hormones in the pills won’t get rid of the cysts, but they can help stop new ones from forming
Surgery is required for some ovarian cysts. That includes those that are significant, persist, or result in symptoms. If you are close to menopause, surgery may also be necessary because cysts are more likely to be malignant at this time.
The surgeon may remove the entire ovary or simply the cyst, depending on your circumstances.
Laparoscopy: For smaller cysts, laparoscopy is used. Above or below your belly button, the doctor creates a very small cut. Your doctor can view inside with the use of tiny camera-equipped equipment, and the cyst or ovary is removed using a separate tool. Most likely, you won’t need to spend the night at the hospital.
Laparotomy: For cysts that could be malignant, laparotomy is used. The belly is sliced more severely throughout the procedure.